Introduction
Naturally occurring novel virus Covid-19 has recognised that human and health security is no longer synonymous with just health sciences. The conception, promotion and care of life (bios) demands an expanded umbrella of health sciences to evolve and institutionalise bio-governance, bio-politics and bio-power, encompassing all domains which potentially bio-marginalise (prevent life to flourish) the human security and well-being. The realm of health security constitutes all endangering factors like natural disasters, outbreaks, pandemics, emerging infectious diseases (EID), misuse of antibiotics leading to unpredictable microbial resistances, critical pharmaceutical, medical supply chain safety, medical and health information cyber-biosecurity, bio-terrorism, climate change, rapid urbanisation, population growth, food security, water security, and social media (SM) misinformation etc, which actively modulate the wellness and health of human populations. A country that blooms and flies high with a vibrant democracy, should have a smart-public health system that provides an ecosystem for its beings to evolve their lives to full potential.
A live, vibrant, ever evolving, flexible, resilient, participatory, engaging public health system must have the well-being of its citizens at its core—a system melting boundaries between different stakeholders, dissolving the idea of segmented hierarchical health system with defined and restricted boundaries at various levels. The boundaries in the health system collage, of participatory responsibilities and accountabilities of all the stakeholders need to dissolve to develop one aesthetic scenery where all merges and gels well with each other at every level of coordination, management and governance. The New India leadership can evolve and embrace this idea of fit, smart and healthy public health systems in India which will take health, wellbeing, and happiness index of nation to the next level. The idea of New India is now to build systems that are lively and which co-evolve with evolving human lives and develop on opportunities instead of breaking at challenges.
This article unfolds various domains with suggestions which may be discussed to develop a futuristic, holistic, comprehensive and integrated public health ecosystem in India. It has suggested a Neuron Model for Public Health Emergency. The author hopes to energise readers to become more aware, active and participatory on issues related to human and health security at local, regional, national, international and global level.
Health first approach
Nation’s well-being must be measured by health (physical, mental and social) of its population, quality of its healthcare policy and programmes, availability of health facilities and qualified and motivated healthcare workforce. Recent epidemic shows the dependency of economic growth and geopolitical status of any country critically on healthcare supremacy. For futuristic nations, health security is one of topmost priority. Health first approach calls for prioritisation of health care structure of any country for present challenges and future risks that incorporates institutionalised comprehensive health policies, scaling up of health care resources, intensive biomedical research, sustainable policies and efficient coordination between stakeholders, with high sense of national priority and commitment.
Establishment of National Institute for Global Health Science and Security:
The institute will conduct courses and research to understand the evolving national and global health challenges. The institute will work in collaboration with the Indian government, international health, agriculture and defence ministries and organisations to collaborate for preparedness for national and transnational disease threats, and develop economic benefits, international security and diplomacy by promoting health research, technologies and services. It will translate research into knowledge products, providing policy analysis and technical support related to the National Health Security, develop research and training for foreign affairs experts on health and research required in global health diplomacy, develop education and training materials for multi-sectoral engagement in the response to biological threats for military and health professionals etc. Courses on global health diplomacy, global health security, emerging infectious diseases, public health management, disease surveillance, bio-safety and biosecurity etc. can be institutionalised as can diploma training in medical and paramedical sciences for developing the human resource and assistance required in rural and primary health care.
Defence Establishment and Participation in Health Security to improve National Capabilities to Prevent, Detect and Respond to Infectious Disease Threats
India’s defence and national security strategy is primarily focused on territorial and border disputes, countering and combating left wing extremism (LWE), insurgency in the North Eastern States and security and stability in Jammu and Kashmir. The non-traditional security threats like pandemics, emerging infectious diseases, and proliferation of Chemical, Biological, Radiological, Nuclear, and high yield Explosives (CBRNE) weapons have to yet find a place in India’s national security strategy, planning and response. Threat of bio-incidents both naturally occurring and manufactured epidemics through the use biological weapon are equally evolving and alarming. Currently, without defined guidelines and protocols on how to address bio-incidents, the counter response and activities rely on ad-hoc responses of questionable utility. The structural and functional gaps between health security, bio-security and bio-defence has caused a damage to human security as we are not able to efficiently harness and incorporate the scientific capabilities, technological innovations for governance and policies related to bio-incidents. India needs to develop a National Biological Security Strategy (NBSS)[1] and National Health Security Act[2] and integrate both in India’s National Security Strategy (NSS) for a comprehensive, holistic biological-socio-economic security approach which addresses threats emanating from both traditional (or military) and non-traditional (or non-military) sources. Post COVID-19, the role of military in national, international and global health security activities can be extended with more extensive networks of bio-intelligence and bio-surveillance, improving the national capabilities to prevent, detect, and respond to natural and simulated bio-incidents.
Establishing a Strict Bio-risk Assessment and Management Guidelines in Health, Veterinary and Agriculture Research to be Complied by all Stakeholders
Bio-safety involves procedures and techniques to prevent an accidental release of bio-agent; biosecurity involves accountability measures and procedures to protect bio-agents from unauthorised access, misuse, thievery for an intentional release. Dual use research that aims to provide knowledge for health security could be misapplied to threaten safety of health, agricultural crops, live stocks and the environment. Without proper guidance, biosafety, biosecurity, and dual use research can become a risk to human life. Life sciences, molecular biology, bio-technology, bio-engineering, genetic engineering, bio-informatics and synthetic biology researches and tools have become common methods in research laboratories[3]. DIY-bio (Do it Yourself Biology), emerging bio-technology program and bio-technology start up are expected to develop futuristic technologies and therapies, but at the same time potential risks of these technologies need to be minimised. Genetically Modified Organisms, gene therapy, induced-Pluripotent Stem Cell (iPS), Gain of Function (GoF) and CRISPR (clusters of regularly interspersed short palindromic repeats) will be star technologies in future providing therapeutic solutions. Futuristic vision of public-health research involves nurturing responsible future generation scientists and developing an effective bio-risk assessment and management guidelines to be complied by all the engaged stakeholders.
Developing Decentralised and Participatory Public Health
Neighbourhood Health Clinics (NCs) should be led by community leaders to complement and micromanage the activities of central-state-district health initiatives[4]. A shift in health governance and policy is required for higher level of micro and higher levels of governance in cities and villages. The local parliament of elected leaders and network of mini health centres at municipality, city council and gram panchayat level will provide a voice and platform for elected leaders, who are often excluded from high-level decision-making to bolster local health capacities. Strong city and village leadership and engagement network is a must for resilient strategic preparedness network.
Expanding the role of Civil Society Organisations (CSOs)
Margaret Chan, Director General, WHO in 2007, highlighted the role of CSOs, stating, “Given the growing complexity of these health and security challenges and the response required, these issues concern not only governments, but also international organisations, civil society and the business community. Recognising this, the World Health Organization is making the world more secure by working in close collaboration with all concerned”. Civil Society Organisations include community-based organisations, non-governmental organisations (NGOs), charitable organisations, labor unions, indigenous groups, faith-based organisations, professional associations, and foundations. With their grassroots presence, CSOs can more effectively help to address health security and health systems challenges and help community resource utilisation in healthcare management. India needs to strengthen CSOs which supplement and fill health systems gaps, enabling governments to micromanage the medical emergency like the Covid-19 outbreak. Prepared CSOs will:
- Support with the establishment of local outbreak response teams for coordinating the national response.
- develop local surveillance and response systems to detect, track and manage disease.
- Manage maintenance of safe health care services (e.g., local isolation centre for patients), educate and train on infection control and prevention procedures.
- Support the administration of vaccines, diagnostic and therapeutics.
- MobiliSe and train to build a wide-range of community health workforce
- Generate finances and resources for response efforts through innovative funding mechanisms.
Strengthening Public Institutions in Fighting Zoonotic Infections and Antimicrobial resistance (AMR)
The basics of preventing deadly epidemics and pandemics involves understanding the origin and dynamics of human-pathogen-animal-environment interactions. Recent infectious diseases like Ebola virus disease, influenza H1N1 and Covid-19 are notably linked to animals such as bat and swine. There is a need to implement one health approach i.e a collaborative, multi-sectoral, and trans-disciplinary approach, working at the local, regional, national, and global levels, with the goal of achieving optimal health outcomes recognising the interconnection between people, animals, plants, and their shared environment[5]. Department of Health Research (DHR) needs to strengthen infrastructure, human resource for health research, research governance, technology development for prevention and management of epidemics/outbreaks. Network of laboratories for surveillance, rapid diagnosis, and effective strategies to neutralise and eventually control and prevent the spread of known/unknown/emerging highly infectious diseases of public & global concern are required. Currently, India has only 2 BSL4 (Bio safety level) facilities—National Institute of Virology (NIV), Pune, and National Institute of High Security Animal Diseases (NIHSAD), Bhopal, for research, diagnosis and control of exotic and emerging animal diseases. Increasing capabilities and re-calibrating the priorities of National Centre for Disease Control (NCDC), Indian Council of Medical Research (ICMR), ICAR-Indian Veterinary Research Institute (IVRI), National Institute of Virology in Pune (NIV) and Defence Research & Development Establishment (DRDE) would help prevent, reduce and prepare with zoonotic infections in the future.
Antimicrobial resistance (AMR) can become the next pandemic as superbugs (bacteria that are resistant to all known antibiotics) will hinder the fight against the many biological infections with our existing range of antibiotics. Collaborative efforts for prudent use antibiotics, preserving the antibiotics that do work, banning medically important antibiotics in food production (three in four antibiotics consumed worldwide are used in food animals), investing in the development of new antibiotics, new treatments for drug-resistant infections can alleviate the AMR crisis.
Harnessing and Integrating Technology and Innovation in Public Health System: Digital Technologies to Improve PHCs
A virus knows no borders, and neither do the digital technologies and data. The penetration and reach of mobile devices have surpassed other infrastructures like electricity, roads and healthcare resources. Mobile devices and networks are present in resource-limited regions where medical infrastructure, equipment and services are unavailable. Public health systems need to align and integrate digital technologies to build online care pathways that rapidly link the widespread diagnosis with digital symptom checkers, contact tracing, epidemiological intelligence and long term clinical followup. With digitalisation of public health systems and integration of advanced technologies, ethical frameworks and systems for storage and analysis, data protection and confidentiality need to be evolved.
Key examples of digital technologies deployed in public-health interventions for the COVID-19[6]
- Machine learning used for Web-based epidemic intelligence tools and online syndromic surveillance
- Survey apps and websites used for Symptom reporting
- Data extraction and visualization used for Data dashboards
- Connected diagnostic device used for Point-of-care diagnosis
- Sensors including wearables used for Febrile symptoms checking
- Machine learning used for medical image analysis
- Smartphone app, low-power Bluetooth technology used for Digital contact tracing
- Mobile-phone-location data used for Mobility-pattern analysis
- Social-media platforms used for Targeted communication
- Online search engine used for Prioritised information
- Chat-bot used for Personalised information
- Tele-conferencing used for telemedicine, referral
Further, post Covid-19, technological intervention can revolutionise the efficacy of traditional health care systems. However, affordability and public access of such technological advancement must be regulated. The prominent technological solutions could be classified as below:
- Precision medicines for individual specific treatment methodologies
- Nanotechnology for target specific drug delivery, efficient sensing and imaging, broad spectrum antibiotics and organ regeneration
- Internet of Medical Things (IoMT) for interconnected communication between biomedical machines, vitals monitors and wearable devices with the help of application and IT infrastructure. This will facilitate virtual interaction patients to their physicians and allowing the transfer of medical data over a secure network.
- Big data for management of healthcare data, genomics and pharmacogenomics data to improve decision-making.
- Block Chain for distributed, decentralised and secured database management system that aims to create digital identification, tracking healthcare related object and secure decentralising database.
- 3D Bio-printing for distantly development of surgical implants, tools, orthopaedic and dental implants.
- Drones for remotely onsite distribution of of drugs, vaccines, blood, plasma and healthcare equipment in accident sites and hilly terrains.
- Robotics for assistance remote controlled precision surgeries assisting medical staff patients in diagnostics and maintaining supply chains.
- Mobile health with micro-fluidic Lab-on-a-Chip technology for rapid diagnosis, better patient monitoring, and spatiotemporal tracking capability.
- One Digital Health ecosystem (National health card for National Health Service digital records). One Nation, One Health and One National Health card for a unified digitally transformed health ecosystem. This will help in understanding the intrinsic complexity of hath care and enable development of novel healthcare solutions.
Expanding the role of Community Health Workers (CHWs)
The traditional roles of CHWs includes health education, routine immunisation, supporting maternal and child health, family planning and reproductive health activities, and surveillance, contact tracing for communicable diseases etc. During Covid-19, in an overwhelming, overstretched health system, CHWs shifted the hospital-centred care to community-centred care. Post Covid-19, recalibration of our future efforts to strengthen resilient public health systems and health emergency preparedness involves expanding and supporting CHWs. CHWs and adequately trained Community Health Volunteers (CHVs) and Village Health Volunteers (VHVs) will facilitate health education including promotion of new normal behaviours, measures to prevent and control virus, assist in surveillance, contact tracing and quarantine and maintain essential health services etc. CHWs need to be recognised as an integral part of the primary health care system and local authorities need to ensure that adequate level of training, resources, incentives and support is allocated to sustain the enthusiasm of CHWs[7].
Transformational leadership willing to pay for public health policies
The effectiveness and performance of a nation’s health system is highly dependent on government leaders as they propose and decide to invest for resources development for public system. Leader’s personality, leadership style, goal alignment, communication skills and team building ability highly influences the public health decisions. Leaders who are future-oriented and who believe in their ability and competence to improve the quality of their society, create more values for future generations and generate more goodwill for society. Reportedly, these leaders tend to invest more in public health to bring well-being and goodwill for their citizens[8]. In addition, positive perceived social support by citizens moderates and drives futuristic leadership model. The politics of difference lies in futuristic investment in public health and the ideal community trust and support the leader’s policy.
Gender Inclusive Engagement Pattern in Health System Governance
Health system governance should be human-centric and barrier-free, inclusive, non-discriminatory with a tailored and targeted response. The social, economic and long-term health consequences, disproportionately impact the lives of women and girls. Taking lessons from Covid-19 response and related health emergencies, a more fair, inclusive, gendered lens is required for health system governance[9].
Development of Private Sector and Donor Participation in Healthcare System
An initiative to involve private sectors, individuals, foreign assistance for collaborative grants, aids, loans, etc, must be modelled to strengthen healthcare infrastructure. The challenges posed by emerging health threats in the 21st century requires collaborative network of cooperation. Appropriate generation and mobilisation of resources requires curbing the corruption, misuse and abuse of financial support and assistance in the health sector. India needs to enhance monitoring measures to ensure effective utilisation of finances and collaboration to prepare and respond to future challenges.
Integration of Ayurveda in Health-care Delivery System
Turning Ayurveda into evidence-based medicine could change the medical philosophy and treatment to an inclusive, affordable, individualised and holistic healthcare. Scientific reliability of Ayurveda, education, research, clinical practice, and public health and administration interventions will facilitate integration with existing public health system. This will help promote health, wellness lifestyle, improve disease prevention and increase access and delivery of health services. An integrated model with preventive, curative, and promotive health care strategy will contribute tremendously in community health.
Value Creation through Next-generation Business Model
Post Covid-19, India needs to develop innovative business models with fresh perspective to observe growth and deliver better care for individuals. The integration of innovation in healthcare model, rewiring of organisations for speed and efficiency and to deliver quality care helping both healthcare players and patients will be needed.
Building a Neuron Model for Public Health Emergency
An integrated model for rapid, defined and efficient reception and communication of response signals among stakeholders to prepare and respond to medical health emergencies is shown in the diagram (Figure 1). The global bio-threats are received by receptor agencies like the WHO, the United Nations Institute for Disarmament Research (UNIDIR), the United Nations Office for Disarmament Affairs (UNODA), Biological Weapon Convention Implementation Support Unit (BWCISU), Indian embassies, information network in cooperation with foreign intelligence agencies, military intelligence, Intelligence bureau, international intelligence units (Bio-intelligence and Bio-surveillance). The information received is processed and risk-assessed by the National Institute for Global Health Sciences and security (NIGHSS), as proposed in this paper) and the Defense Research Laboratory (DRL, BSL-4 Level, to be developed as proposed in this paper). The information and drafts guideline, according to threat and risk assessment, is received by the central decision command headed by the Prime Minister and which includes as its members, the Defense Minister, Minister of External Affairs, National Security Advisor (NSA), Chief of Defence Staff (CDS), and the three Service Chiefs. The decision made by the central decision command is communicated to President, the three Service Chiefs, Parliamentary Committees, leader of opposition, state governors, cabinet & ministers, planning commission, and regulating agencies to broadcast information to coordinate market for supply, production and distribution of drugs and life support systems efficiently, using big data management system, block chain technology etc.
Receiving the information, the state governments coordinates and functions with district and community stakeholders for delivery of efficient governance, using technologies like Internet of Medical Things (IoMT), telecommunication, block chain technology, e-consultation, drones & robotics etc. The neuronal communication is bidirectional i.e. reception of signal, and delivery of response from top to bottom or bottom to top is as per the stimulus (information) available. All the bio-health data will be collected in mega National Biomedical Database (depository for pathological, pharmacological, genomic, serological toxico genomics data) for efficient tracking and feedback system in the proposed neuron model.
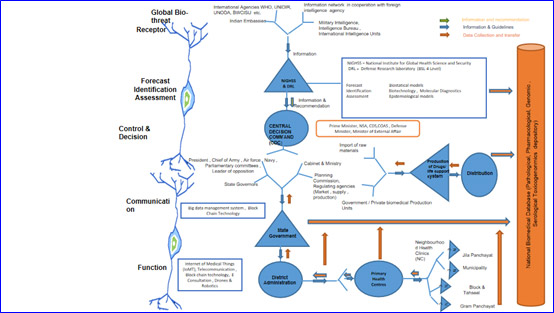
Figure 1: Neuron Model for Public Health Emergency
Conclusion
“It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness, it was the epoch of belief, it was the epoch of incredulity, it was the season of light, it was the season of darkness, it was the spring of hope, it was the winter of despair.”- Charles Dickens.
Covid-19 has expanded the understanding and redefined the scope of public health system and community. During the pandemic, the world embraced a holistic approach of health security, an area which was traditionally seen with myopic vision and scope. The global engagements to ensure public health cooperation, interconnectedness between science, public health, international economics, politics and policy are now understood to be important areas of public health. Hence, the public health apparatus must be equipped with comprehensive and integrated, proactive governance measures which recognise all the dimensions and respond to the evolving health challenges. Post Covid-19, public health systems need to return with a respect and responsibility towards life’s existence with a fully functioning inclusive healthcare system with evolved work processes and strengthened institutions beyond inequalities, and discriminatory hierarchies. The core strength of public health system lies in strengthening traditional aspects of public health such as hygiene, disease detection and prevention measures, screening and immunisation and health promotion in national programme. These strengthened resources and frameworsk like diagnostic centre, surveillance measures and immunisation networks for national programme for preventable diseases like tuberculosis, polio, measles etc can be repurposed for unseen outbreak of infectious diseases.
Coming back stronger, India needs to generate the vision for a lively public healthcare ecosystem which dynamically evolves, adapts, lives, acts and complies to modern society and brings the triumph of the human spirit.
Author Brief Bio: Dr Aakansha Bhawsar is a Scientist at the Division of Basic Medical Sciences, Indian Council of Medical Research (ICMR), Headquarters in New Delhi.
References:
[1] https://chintan.indiafoundation.in/articles/national-biological-security-strategy-a-way-forward/
[2] https://chintan.indiafoundation.in/articles/india-needs-national-health-security-act/
[3] https://indiafoundation.in/articles-and-commentaries/science-of-biological-warfare-and-biopreparedness/
[4] https://chintan.indiafoundation.in/articles/neighborhood-health-clinics-an-improvised-and-micromanaged-model-for-evolving-local-bodies-led-neighborhood-clinics-in-india/
[5] https://www.cdc.gov/onehealth/basics/index.html
[6] Budd, J., Miller, B.S., Manning, E.M. et al. Digital technologies in the public-health response to COVID-19. Nat Med 26, 1183–1192 (2020). https://doi.org/10.1038/s41591-020-1011-4
[7] Supriya Bezbaruah, Polly Wallace, Masahiro Zakoji, Wagawatta Liyanage, Sugandhika Padmini Perera, Masaya Kato, Roles of community health workers in advancing health security and resilient health systems: emerging lessons from the COVID-19 response in the South-East Asia Region, WHO South-East Asia Journal of Public Health, 2021, Volume 10, Issue 3, Page 41-48.
[8] Wang J, Chou TP, Chen CP, Bu X. Leaders’ Future Orientation and Public Health Investment Intention: A Moderated Mediation Model of Self-Efficacy and Perceived Social Support. Int J Environ Res Public Health. 2020;17(18):6922. Published 2020 Sep 22. doi:10.3390/ijerph17186922
[9] https://chintan.indiafoundation.in/articles/rethinking-a-gender-inclusive-engagement-pattern-in-health-system-governance/